Translate this page into:
Sociodemographic Characteristics and Clinical Profile of Inpatients in the Psychiatry Unit of a Tertiary Care Hospital in Assam: A Retrospective Study
*Corresponding author: Dr. Porineeta Gogoi, Department of Psychiatry, Assam Medical College and Hospital, Dibrugarh, India. porineetagogoi95@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bora K, Gogoi P, Gogoi A, Chauhan N. Sociodemographic Characteristics and Clinical Profile of Inpatients in the Psychiatry Unit of a Tertiary Care Hospital in Assam: A Retrospective Study. Acad Bull Ment Health. 2024;2:36-41. doi: 10.25259/ABMH_10_2024
Abstract
Objectives
Recent years have seen a significant evolution in the understanding pertaining to mental health issues. The analysis of the intricate interplay between an individual’s sociodemographic factors, genetic makeup, the environment, and clinical profile (diagnosis and treatment) of patients will help us understand the prevalence and types of mental health disorders prevalent in Assam, which is a culturally, ethnically and socially diverse state. The pattern of utilization of electroconvulsive therapy has also been analyzed. The aims and objectives of the study is to analyze the sociodemographic characteristics and clinical profile of patients admitted in Psychiatry ward, Assam Medical College and Hospital.
Material and Methods
An analysis on the case records of all individuals admitted to the hospital’s Psychiatry ward between August 1, 2022 and July 31, 2023 was done. Data on socio-demographic details such as age, gender, domicile and clinical profile (diagnosis, mode of discharge, duration of stay and treatment) was compiled using semi-structured format designed by authors. Information regarding patients undergoing electroconvulsive therapy was also gathered from the records. Statistical analysis: The data were subjected to analysis utilizing the Statistical Package for Social Sciences (IBM SPSS Statistics for Windows, version 25.0).
Results
A total of 680 patients got admitted of which higher proportion constituted of male (77.58%) and majority individuals were aged between 30 and 39 years (29.65%). The predominant diagnosis among the inpatients was substance use disorders (39.09%). Out of all the psychotropic drugs, olanzapine (17.94%) was mostly prescribed on discharged followed by risperidone (10.15%). Escitalopram (3.97%) was the mostly prescribed antidepressant on discharge. Patients diagnosed as substance use disorders were mostly discharged on lorazepam (5%), baclofen (14.26%) and received an average number of 1.8 sessions of Motivational Enhancement Therapy (MET). Whereas, schizophrenia and related disorders was the most common diagnosis among inpatients receiving ECT (51.52%).
Conclusion
Our study helped to understand the socio-demographic attributes and clinical profile of the inpatients to foster better management approaches.
Keywords
Mental health
mental hospitals
electroconvulsive therapy
inpatient service
substance use
INTRODUCTION
Mental disorders encompass a broad spectrum of conditions that impact an individual’s thoughts, emotions, and behavior. These disorders can manifest in various forms, impacting people of all ages and backgrounds. With a substantial prevalence, mental health issues are seen to contribute to widespread morbidity, diminished quality of life, and considerable socioeconomic consequences impacting individuals and society at large. These disorders contribute to a substantial portion of Disability Adjusted Life Years (DALYs) globally, with India alone representing 15% of these DALYs.[1]
It has been observed that the number of psychiatry patients requiring admission has been increasing every year. Psychiatry inpatient services are crucial for assessing, treating, and stabilizing individuals with severe psychiatric conditions. This plays a pivotal role in managing acute symptoms, ensuring safety, and establishing a foundation for ongoing patient care. The history of the development of mental hospitals globally reveals a progression from early establishments in Byzantium and Jerusalem to the modern Bethlem Royal Hospital in London in 1247.[2,3] Over the centuries, the focus shifted from humane care in hospitals to concerns about poor patient conditions, prompting initiatives like Pinel’s “moral treatment” and Dorothea Dix’s efforts in the 19th century.[4,5] In India, the establishment of mental hospitals can be linked to the era of lunatic asylums, influenced by British and European ideologies, with historical documentation dating back to the rule of Md. Khilji. Preceding this era, instances of tending to mentally ill patients were noted in temples and religious institutions in South India.[6] The 1857 revolution’s suppression in 1858 facilitated a power transfer to the Crown, accompanied by the inaugural Lunacy Act (Act no. 36). The transition from mental asylum to mental hospital signifies a broader cultural recognition of the importance of treating mental health with dignity and compassion rather than isolating patients from the community, which was contrary to the stigmatizing perception of mental illness. Yet, mental health institutions in India, like in many other nations, grapple with social challenges, inequalities, and limited resources in terms of personnel and financial investments for providing inpatient services.
A National Mental Health Survey (NMHS) conducted by the National Institute of Mental Health and Neurosciences (NIMHANS) in 2016 shows a heightened risk for mental morbidity among males aged 40–49 years and in socially deprived segments of Indian society, which highlights the role of sociodemographic correlates in psychiatric morbidities.[7] However, treatment-seeking in psychiatric patients relies on numerous factors like service availability, stigma, community participation, traditional healing practices, transportation, comorbid health conditions, and many additional factors. The 2016 NMHS noted that merely two out of ten individuals affected by mental illness reported receiving any formal mental health care, resulting in a treatment gap of 84.5%.[7] Despite the need for long-term inpatient care in mental hospitals, factors such as stigma, distrust in the mental health system, financial concerns, and lack of insight contribute to a decline in psychiatric admissions. The lack of epidemiological data regarding mental morbidities may be a contributing factor to the gap in treatment-seeking.
The clinical profile provides crucial insights into the diagnosis, mode of discharge, duration of stay, and treatment methods, shaping the prevalence, presentation, and management of psychiatric conditions. Additionally, understanding various medications administered upon discharge is crucial as it sheds light on post hospitalization care practices and their impact on patient outcomes. The study also examines electroconvulsive therapy (ECT) as a treatment option in psychiatry inpatients in this region of India, data of whom was limited.
Therefore, a study was conducted to examine sociodemographic attributes and clinical profiles of inpatients, aiming to fill knowledge gaps regarding mental health issues of hospitalized patients in Northeast India. However, a concise discussion and critical assessment has also been conducted on various factors that could impact the admission rate and hinder treatment-seeking. This will ultimately help in the implementation of measures for preventing and treating psychiatric morbidities and to reduce barriers in seeking mental health care by adding to the scant epidemiological data from this region.
MATERIAL AND METHODS
This was a retrospective study conducted at the Department of Psychiatry, Assam Medical College and Hospital, Dibrugarh, Assam, based in a hospital setting, which operates autonomously and is equipped to offer psychiatric care to both inpatients and outpatients. The study included secondary data of patients contained in the admission register who attended the Psychiatry Department, Assam Medical College and Hospital and were subsequently admitted as inpatients for treatment from August 1, 2022, to July 31, 2023. The diagnosis was determined based on the outline in the tenth edition of the International Classification of Diseases (ICD-10).
Data were collected from the admission register in the Psychiatry Ward. The record of patients with inadequate information was excluded. A specific format was employed to direct the gathering of data from patient’s records. It included details of inpatients pertaining to sociodemographic factors such as age, gender, and domicile that were gathered. Clinical profile details such as diagnosis, mode of discharge, and duration of stay and treatment (both pharmacological and nonpharmacological) were recorded digitally. Data regarding sociodemographic correlates of patients receiving ECT was also gathered from the maintained records. The data set also encompassed readmissions. Data analysis was done by computing mean, standard deviation, and percentage profiles utilizing the Statistical Package for Social Sciences (IBM SPSS Statistics for Windows, version 25.0).
RESULTS
A total of 680 (526 male and 154 female) patients got admitted between August 1, 2022, and July 31, 2023, in the Psychiatry Department, Assam Medical College and Hospital. It was observed from Table 1 that the highest admission was seen in the 30–39 years age group (29.65%). The majority were males (77.58%) and from urban backgrounds (52.06%).
| Parameters | Number (%) | |
|---|---|---|
| Age-group (years) | <20 | 70 (10.29) |
| 20–29 | 171 (25.15) | |
| 30–39 | 201 (29.56) | |
| 40–49 | 148 (21.76) | |
| 50–59 | 63 (9.26) | |
| >60 | 27 (3.97) | |
| Gender | Male | 526 (77.35) |
| Female | 154 (22.65) | |
| Domicile | Rural | 326 (47.94) |
| Urban | 354 (52.06) | |
In Table 2, the average length of hospitalization was observed to be 14.07 days (SD = 12.19).
| Parameters | Number (%) | |
|---|---|---|
| Diagnosis (according to ICD-10) | F10–F19 | 264 (38.82) |
| F20–F29 | 218 (32.06) | |
| F30–F39 | 60 (8.82) | |
| F40–F48 | 47 (6.91) | |
| F50–F59 | 2 (0.29) | |
| F70–F79 | 4 (0.59) | |
| F80–F84 | 1 (0.15) | |
| G40 | 5 (0.74) | |
| Others | 35 (5.15) | |
| Mode of discharge | Absconded | 22 (3.24) |
| Discharge against medical advice | 70 (10.29) | |
| Discharge on advice | 427 (62.79) | |
| Discharge on disciplinary ground | 19 (2.79) | |
| Discharge on request | 78 (11.47) | |
| Leave against medical advice | 23 (3.38) | |
| Shifted to other department | 16 (2.35) | |
ICD-10: The tenth edition of the International Classification of Diseases (ICD-10)
Table 3 reveals that the majority of the inpatients (39.09%) were diagnosed as substance use disorders (F10–F19 according to ICD-10), where males comprised 37.94% of the total population. The mode of discharge varied, but mostly 428 patients (63.13%) were discharged on advice, and 15 patients (2.21%) were referred to other departments. It was also observed in Figure 1 that the predominantly prescribed psychotropic drug on discharge was olanzapine (17.94%) followed by risperidone (10.15%). Antidepressants like escitalopram (27%) and fluoxetine (12%) were also prescribed. Patients diagnosed with substance use disorders were mostly discharged on lorazepam (5%) and baclofen (14.26%) out of all psychotropic drugs.
| Duration of stay | Mean | SD |
|---|---|---|
| Duration (day) | 14.20 | 12.20 |
SD—standard deviation
Table 4 shows that 33 patients (25 males and 8 females) received ECT in the study period. The majority belonged to the 20–29 years age group (42.42%) and were males (75.76%). Among inpatients receiving ECT, schizophrenia and related disorders were the predominant diagnosis (51.52%) and the average number of ECT sessions was 4.45 (SD = 2.61).
| Parameters | Number (%) | |
|---|---|---|
| Age-group (years) | <20 | 4 (12.12) |
| 20–29 | 14 (42.42) | |
| 30–39 | 8 (24.24) | |
| 40–49 | 5 (15.15) | |
| 50–59 | 2 (6.06) | |
| Gender | Male | 25 (75.76) |
| Female | 8 (24.24) | |
| Diagnosis (according to ICD-10) | Schizophrenia | 18 (64.28) |
| Mood (affective) disorders | 10 (30.30) | |
| ECT | Mean | SD* |
| 4.45 | 2.61 | |
DISCUSSION
Numerous epidemiological investigations carried out in Asia indicate that around 680 million people face the potential of developing mental health conditions, significantly affecting their quality of life. This study was conducted to assess sociodemographic factors like age, gender, and domicile. The clinical profile and treatment received among admitted patients in the psychiatry department within a tertiary care hospital located in Northeast India were evaluated to study the trend for formulating effective management approaches.
Our study shows peak admission in the age range of 30–39 years, the majority being males. The age-wise distribution of inpatients indicates a concentration of cases among individuals aged 20–49 years. This underscores the importance of targeted healthcare interventions for this productive age group and reflects various factors contributing to mental health issues within this demographic, including socioeconomic stressors, work-life imbalance, relationship strain, co-occurring disorders like substance abuse, life transitions, and barriers to accessing mental healthcare due to stigma. Addressing these factors is essential for providing effective psychiatric care tailored to the specific needs of this age group. This observation aligns with the results reported by Mudgal V et al.[8] It was also revealed that psychiatric disorders affect individuals in the prime of their productive years, often affecting the younger population.[9] However, the mean age of indoor patients indicates variability of ages in our study.
Earlier research has underscored that the female gender is notably prominent among the risk factors associated with psychiatric morbidities.[10,11] Our study revealed a significant gender disparity, with a higher representation of male patients (77.58%) compared to females (22.71%), similar to a study by Chaudhury et al.[12] The stigma surrounding mental health care, deeply rooted cultural expectations, perception of the need for professional intervention, and availability of healthcare resources might be factors attributing to these findings. Also, a paternalistic society may hinder women from seeking assistance for mental health issues by restricting their ability to go outside.[13] This imbalance underscores the need for further exploration into the factors for the development of gender-specific interventions and support services.
Among the study population, 52.06% of inpatients were reported as residing in urban areas, whereas 47.94% were from rural areas. Ghosh P et al. (2019) also demonstrated similar results.[14] The possible reasons may be easy access to services, greater awareness, and socio-economic factors influencing treatment-seeking among the urban population. This raises a need to create awareness among the rural population.
The majority of patients (39.09%) admitted to the psychiatry ward in our study have substance use disorders. Observations revealed that alcohol was the most commonly used substance among the inpatients (82.29%). This could be because of the availability of management options for the treatment of substance use disorders. The highest prevalence of substance use disorders was observed in the age group of 30–39 years, followed by the 40–49 years age group. This reflects the typical age range for the onset and peak of substance use disorders, often associated with social and environmental factors such as peer influence, stressors related to work and family, and accessibility to substances. Whereas in a study by Kena T et al., the majority of patients were diagnosed with opioid dependence (77.62%).[15] In our study, schizophrenia, schizotypal, and delusional disorders represented the second most prevalent diagnoses (32.15%), followed by mood disorders (8.85%), which was in contrast to the findings of other studies.[16,17] Cultural factors could account for the variation in the observed morbidity pattern.[14]
Literature suggests schizophrenia typically manifests in late adolescence or early adulthood, which can be supported by the findings in our study, where the highest occurrence was identified in the 20–29 years age group. Advancements in neuroimaging research have investigated the patterns of brain alterations that occur during typical development and in conjunction with the emergence of psychopathological conditions.[18] Another potential explanation may be attributed to the recognition and diagnosis of the disorder during these formative years. Prevalence of mood disorders seemed to peak in the 20–29 years age-group, with a notable decline in older age groups; the latter may be due to effective treatment or remission of symptoms. Moreover, underreporting in older populations cannot be overruled.
The analysis highlighted mode of discharge, notably showing 63.13% being discharged on advice. Additionally, 11.50% requested discharge voluntarily, while 10.47% left against medical advice, with other methods for the rest. And the average duration of stay was 14.20 days, which plausibly explains the admission policies. In our study, 3.24% of the inpatients absconded, similar to another study by Gowda G. et al.[19]
The study also emphasizes on the diverse range of medications being prescribed on discharge, with olanzapine being the most frequently prescribed antipsychotic (48.99%), followed by risperidone (27.7%); the least prescribed antipsychotic was amisulpride (3.6%). Other antipsychotics, such as aripiprazole, quetiapine, and chlorpromazine, were also prescribed. The most prescribed antidepressant on discharge was escitalopram (62.79%) followed by fluoxetine (27.9%) and paroxetine (9.3%). The patients received an average of 15 mg of olanzapine, 4 mg of risperidone, and 10 mg of escitalopram on discharge. Baclofen was seen to be the most frequently prescribed anti-craving medication (78.86%). Acamprosate follows a moderate prescription frequency of 16.26%, while naltrexone has a relatively low prescription rate at 4.87%, which indicates their underutilization or lesser preference among prescribers. These findings were similar to another study.[20]
However, data on inpatients receiving nonpharmacological treatment revealed the majority as males belonging to the age–group of 20–39 years and diagnosed with substance use disorders. They received an average of 3.5 sessions of Motivational Enhancement Therapy (MET). Patients who underwent psychological intervention alongside appeared to exhibit improved response rates. Various studies also advocate for integrating pharmacological and psychological for psychiatric disorders.[21,22] Other psychological interventions administered include counseling, Cognitive Behavioral Therapy (CBT), relaxation techniques, and psychodiagnostic tests, with an average of 3.9 sessions.
ECT plays a crucial role in the treatment of psychiatric patients, especially those with persistent psychotic symptoms who have not responded well to multiple trials of antipsychotic medications, including clozapine. Our analysis indicated that a majority of individuals receiving ECT fell within the age range of 20–39 years, potentially reflecting a higher prevalence of severe psychiatric conditions, such as treatment-resistant schizophrenia or mood disorders in this age group. Another notable observation revealed that a significantly higher percentage of male patients (75.76%) received ECT compared to their female counterparts (24.24%). This discrepancy might be explained by cultural or societal factors. The predominant diagnosis among ECT inpatients was schizophrenia and related disorders (51.52%), followed by affective disorders (30.3%), similar to the findings of Grover et al.[23]
Our study indicates a higher proportion of inpatients with substance use disorder which highlights the importance of addressing these issues in health professional education, in-patient resources, and service planning to improve healthcare delivery. More studies from this region of India will help formulate ward design. Above all, it’s crucial to enhance the hospital staff and provide training for effective management of inpatients, which will be possible by the availability of epidemiological data.[24,25] Training staff in psychosocial intervention is also equally important.[26,27]
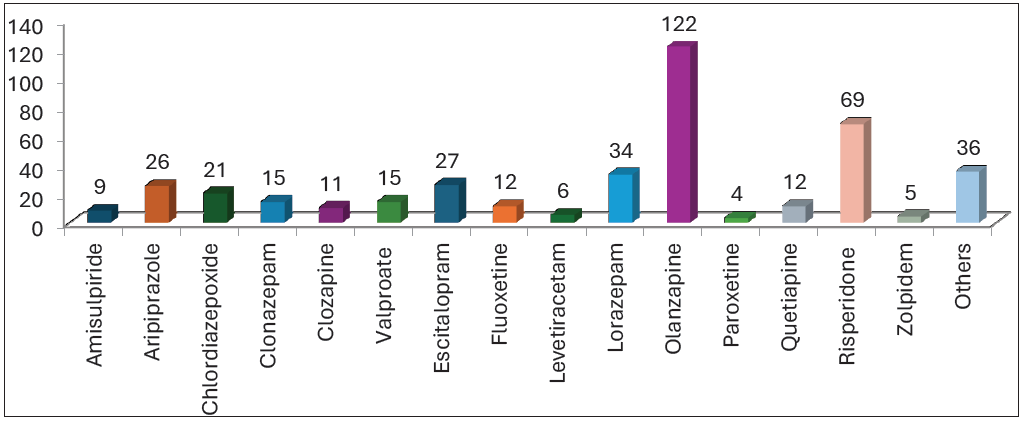
- Medication received by psychiatry inpatients during discharge.
LIMITATIONS
It was a retrospective study that could not track changes of morbidity over time, considering the dynamic nature of psychiatric disorders. Furthermore, since the study was conducted in a hospital setting, the findings may not be generalized to the broader community. Third, data was acquired from the indoor admission register, failing to provide the whole information.
CONCLUSION
Our study highlights the various sociodemographic correlates and the clinical profile of patients admitted to the tertiary care hospital. Additionally, it identifies sociodemographic attributes of inpatients undergoing ECT.
Understanding these characteristics, clinical profile and treatment received not only aids in designing interventions but also contributes to the formulation of successful public health approaches targeting prevention and early intervention. As we delve deeper into the complexities of mental health and with the addition of more data from this region of India, the understanding will lay the groundwork for promoting a more empathetic and knowledgeable approach to psychiatric care.
Ethical approval
The research/study approved by the Institutional Ethics Committee of Assam Medical College and Hospital, number AMC/EC/1939, dated 13th May 2024.
Declaration of patient consent
Patients consent not required as there are no patients in this study. Information was not collected directly from patients. Hence consent from the patient was not required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- The Burden of Mental, Neurological, and Substance use Disorders in China and India: A Systematic Analysis of Community Representative Epidemiological Studies. Lancet. 2016;388:376-89.
- [CrossRef] [PubMed] [Google Scholar]
- The History of Modern Psychiatry in India. Hist Psychiatry. 2001;12:431-58.
- [CrossRef] [PubMed] [Google Scholar]
- History of Mental Hospitals in the Indian Sub-continent. Indian J Psychiatry. 1984;26:295-300.
- [PubMed] [PubMed Central] [Google Scholar]
- The Mental Health System in India History, Current System, and Prospects. Int J Law Psychiatry. 2000;23:393-402.
- [CrossRef] [PubMed] [Google Scholar]
- The National Mental Health Survey of India (2016): Prevalence, Socio-demographic Correlates and Treatment Gap of Mental Morbidity. Int J Soc Psychiatry. 2020;66:361-72.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern, Clinical and Demographic Profile of Inpatient Psychiatry Referrals in a Tertiary Care Teaching Hospital: A Descriptive Study. Gen Psychiatr. 2020;33:e100177.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and Age Of-onset Distributions of DSM IV Mental Disorders and Their Severity Among School Going Omani Adolescents and Youths: WMH-CIDI Findings. Child Adol Psych Ment Health. 2009;3:29.
- [Google Scholar]
- Gender and Mental Health: Do Women have more Psychopathology, Men more, or both the Same (and Why)? In: Horwitz AV, Scheid TL, eds. A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York, NY, US: Cambridge University Press; 1999. p. :348-60.
- [Google Scholar]
- Psychiatric Morbidity Among Patients Attending Medical Outpatient Department. Ind J Psychiat. 1986;28:139.
- [Google Scholar]
- Psychiatric Emergency Referrals in a Tertiary Care Hospital. Med J DY Patil Vidyapeeth. 2018;11:312.
- [Google Scholar]
- Cultural Norms Versus State Law in Treating Incest: A Suggested Model for Arab Families. Child Abuse Negl. 2003;27:109-23.
- [CrossRef] [PubMed] [Google Scholar]
- The Sociodemographic and Clinical Profile of Patients Attending a Private Psychiatry Clinic in Assam, India. Ind J Priv Psychiatry. 2019;13:52-7.
- [Google Scholar]
- Patterns of Psychiatric Illness in a Tertiary Care Centre of Arunachal Pradesh: An Observational Study. Maedica (Bucur). 2022;17:628-35.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Prospective Analysis of 300 Cases Attending Outpatient Clinic in Mental Hospital. In: Proceedings of the Workshop on National Mental Health Planning, Kathmandu. 1987. p. :47-73.
- [Google Scholar]
- District Mental Health Programme in India: A Study of Socio-Demographic and Clinical Data of Patients Attending DMHP Dumka (Jharkhand) Int J Sci Res. 2017;6:13-16.
- [Google Scholar]
- Age of Onset of Schizophrenia: Perspectives from Structural Neuroimaging Studies. Schizophr Bull. 2011;37:504-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and Clinical and Coercion Characteristics of Patients Who Abscond During Inpatient Care from Psychiatric Hospital. Indian J Psychol Med. 2019;41:144-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Drug Utilization Study of Psychotropic Drugs in Indoor Patients of Psychiatry Department in a Tertiary Care Hospital. Annals of Indian Psychiatry. 2020;4:175-80.
- [Google Scholar]
- Application of Motivational Enhancement Therapy in Group Settings Among Patients with Substance Abuse. Indian J Psychiatr Soc Work. 2019;10
- [Google Scholar]
- Efficacy of Psychosocial Interventions for Mental Health Outcomes in Low-Income and Middle-Income Countries: An Umbrella Overview. Lancet Psychiatry. 2020;7:162-72.
- [CrossRef] [PubMed] [Google Scholar]
- The Clinical Profile and Outcome of Patients Receiving Continuation Electroconvulsive Therapy (C-ECT): A Retrospective Study. Indian J Psychiatry. 2023;65:647-54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Management of Adults Recovering from Alcohol or Other Drug Problems: Relapse Prevention in Primary Care. JAMA. 1998;279:1227-31.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Hospital Care: Ineffective, Inefficient and Poorly Organised. Psychiatr Bull. 1999;23:257-9.
- [Google Scholar]
- Screening, Brief Intervention and Referral to Treatment (SBIRT): Toward a Public Health Approach to the Management of Substance Abuse. Subst Abus. 2007;28:7-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dual Diagnosis of Severe Mental Illness and Substance Misuse: A Case for Specialist Services? Br J Psychiatry. 1997;171:205-8.
- [CrossRef] [PubMed] [Google Scholar]