Translate this page into:
Assessment and Management of Depressive Disorder: A Case Report of an Unmarried Adult
*Corresponding author: Dr. Addah Temple Tamuno-opubo, Faculty of Social Science, Department of Psychology, Obafemi Awolowo University, Ile-Ife, Osun State, Nigeria. addahson5@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tamuno-opubo TA, Olusayo AO, Obaniyi JO. Assessment and Management of Depressive Disorder: A Case Report of an Unmarried Adult. Acad Bull Ment Health. doi: 10.25259/ABMH_22_2024
Abstract
This case study examines the psychological and social aspects impacting the mental well-being of a 32-year-old unmarried woman. Based on comprehensive clinical assessment, Client D.A. was diagnosed with Major Depressive Disorder (MDD) using Structured Clinical Interview for DSM-5 (SCID-5), Minnesota Multiphasic Personality Inventory (MMPI-2), Rotter Incomplete Sentences Blank College Form (RISB), Draw-a-Person (DAP), clinical interviews, and behavioral observations. A multifaceted treatment plan was developed, combining cognitive behavioral therapy (CBT), interpersonal therapy (IPT), pharmacotherapy, mindfulness, and relaxation techniques. This study provides insights into her experiences of depression, social isolation, societal expectations, and self-esteem. Over the course of the treatment, Client D.A. demonstrated significant improvement in her depressive symptoms. Her negative thought patterns were effectively restructured through CBT and her interpersonal relationships improved with IPT. Additionally, pharmacotherapy stabilized her mood, while mindfulness techniques helped manage anxiety and stress. This case study highlights the complex interplay of factors influencing mental health and underscores the importance of culturally sensitive, personalized treatment approaches, as evidenced by Client D.A.’s increased social engagement, reduced loneliness, and improved well-being, with regular evaluations confirming sustained progress and the efficacy of the integrated treatment plan in promoting recovery.
Keywords
Adult
Assessment
Depression
Mental well-being
Treatment
Unmarried
INTRODUCTION
Depression is a multifaceted and pervasive mental health disorder affecting millions globally, cutting across age, gender, socioeconomic status, and cultural backgrounds.[1,2] Characterized by sustained feelings of sadness, hopelessness, and a lack of interest in daily activities, depression can profoundly impede an individual’s cognitive, emotional, and physical functioning.[3,4] According to Zwart,[5] the ramifications of untreated depression are far-reaching, impacting not only the affected individuals but also families, communities, and society at large. With a diverse spectrum of symptoms and severities, depression presents a unique challenge to healthcare professionals, researchers, and policy-makers alike. This assessment report endeavors to comprehensively examine the current state of depression, delving into its causes, manifestations, comorbidities, and available interventions.
Feelings of isolation considerably aggravated client D.A.’s mental distress, further exacerbated by the perception that she is being judged by both her peers and family.[6–8] This perspective provides a striking illustration of the intricate relationship between the psychological constructs of individuals and the larger norms and expectations of society. By synthesizing modern research findings and clinical practices, the objective is to promote a deeper understanding and provide insights that can be implemented to improve diagnosis, treatment, and prevention efficiency. This case study explores the progression of treatment for Client D.A., incorporating both psychotherapeutic and pharmacological interventions. Progress was measured through validated scales and client feedback over the course of the therapy.
CASE REPORT
Client D.A. is a 32-year-old unmarried female who has been experiencing significant stress for two years. She traced the onset of her symptoms to August 2021, when she reconciled with a former partner and took out multiple loans to financially support him. Her partner ended the relationship abruptly, leaving her solely responsible for the debt while also caring for her sick mother and preparing for an employment examination. Her partner then got engaged, married another person, and relocated overseas. Approximately 14 months later, Client D.A. entered a relationship with an old friend who visited the country briefly; this relationship also ended abruptly when her partner relocated abroad without informing her. These stressful life events, combined with financial pressure, led her to contemplate suicide multiple times. Client D.A. reported significant complaints, including loss of interest in previously enjoyed activities, poor concentration, low self-esteem, frequent panic attacks, defensiveness, poor personal hygiene, and prolonged sleeplessness lasting several days at a time. She took clonazepam (sold under the brand name klonopin), a benzodiazepine recommended by a friend, to manage her symptoms and reported that the medication was somewhat helpful for over five months.
Further inquiries into her history revealed that she comes from a polygamous family with four wives, where her mother was the first wife. Her father, Mr. D.S., is a 58-year-old accountant and Bursar with a Master’s degree, and her mother, Mrs. Z.A., is a 55-year-old trader who attended Nigeria Teacher’s Institute. Client D.A. has two siblings: a 27-year-old male public servant and a 21-year-old female corps member. She reported that her pregnancy was full term, though her mother experienced prolonged labor about seven days,[9] and D.A. was born with jaundice and placed in an incubator. Developmental milestones were normal, but she stopped breastfeeding at three months due to her mother’s work commitments. She described her relationship with her parents and siblings as cordial but noted being unfairly blamed during her childhood, contributing to her current low self-esteem and stress level.[10] Client D.A., identified as female, is not currently in a relationship, stating that her desire for sex is absent. She holds a Master’s degree in Accounting and is a Certified Fraud Examiner. She has undergone surgery for appendicitis and treatment for a liver infection, with no psychiatric issues reported during childhood or adolescence. Before the onset of her symptoms, she was cheerful, had hobbies such as writing, reading, and sewing, was optimistic about life’s pursuits, was involved in the lives of family and friends, and was always eager to learn and grow.
Assessment
The clinical interview and history provided a thorough overview of Client D.A.’s presenting symptoms, significant life events, and major impairments caused by her difficulties. The interview covered how she coped with her symptoms, any prior medical, psychological, or psychiatric help sought, her beliefs about her issues, her attitude toward these difficulties, and her cognitive functioning and mood at the time. Additionally, information was gathered on her family history, early development, educational history, psychosexual history, occupational history, and subjective ratings of her presenting complaints.[11–12] During the interview, Client D.A. exhibited a range of depressive symptoms, including low mood, anhedonia, disrupted sleep patterns, changes in appetite, and persistent feelings of worthlessness. Her affect was congruent with her reported mood, and she displayed psychomotor agitation. Based on the clinical interview and the presentation of symptoms, Client D.A. met the criteria for Major Depressive Disorder (MDD), DSM-5 code 296.33 (recurrent, moderate). Further assessment, including the Minnesota Multiphasic Personality Inventory (MMPI-2), Rotter Incomplete Sentences Blank College Form (RISB), and Draw-A-Person (DAP) test, was warranted to rule out other potential contributors.
Given Client D.A.’s cultural background, particular attention was paid to culturally sensitive practices throughout therapy. For instance, therapeutic interventions were adapted to respect her family dynamics and cultural values, especially during interpersonal therapy (IPT) sessions, where family relationships played a key role. This ensured that the treatment aligned with her cultural beliefs and social context. As illustrated in Figure 1, Client D.A.’s risk factors included prolonged social isolation and unaddressed emotional trauma, while protective factors such as family support and willingness to engage in therapy was key to her recovery. Figure 2 outlines the cognitive model used to formulate her depressive symptoms, linking her distorted thoughts to behavioral and emotional consequences. These visual aids were presented during the initial sessions to help the client understand the formulation of her depression and guide therapeutic interventions.
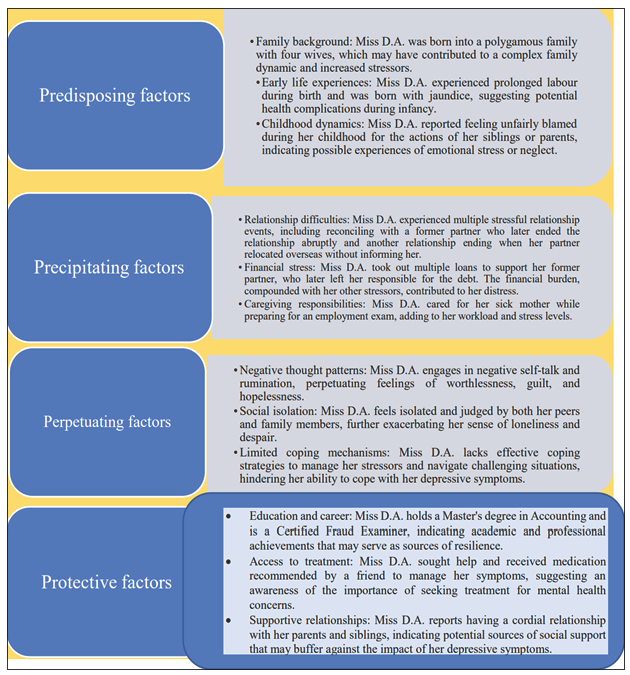
- Client’s risk and protective factors.
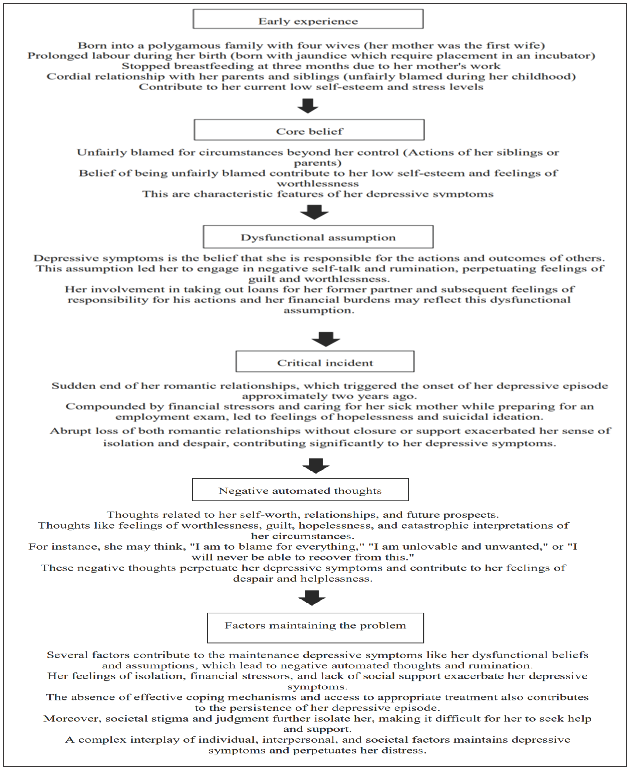
- Client’s problem was formulated based on the cognitive model.
Measurement
Structured clinical interviews for DSM-5 disorders: The Structured Clinical Interview for DSM-5 (SCID-5), developed by The American Psychiatric Association[13] was utilized to diagnose MDD based on DSM-5 criteria. Mental health professionals widely use this semi-structured diagnostic interview to assess and diagnose psychiatric disorders, including mood disorders, anxiety disorders, psychotic disorders, and substance use disorders. The SCID-5 assesses both current and lifetime diagnoses of depression, providing a comprehensive evaluation of an individual’s clinical presentation across multiple axes, such as Axis I (clinical illnesses) and Axis II (personality disorders and intellectual disabilities). The administration of the SCID-5 takes approximately 10–15 minutes to complete the questionnaire, ensuring a thorough assessment of the specific criteria for each condition.
During the structured administration of the SCID-5 for MDD, each diagnostic criterion was systematically explored, allowing for an in-depth assessment of the nature, duration, and impact of the depressive symptoms experienced by Client D.A. The interview covered the severity of depressive symptoms, categorizing them as mild/moderate/severe based on the responses and overall clinical presentation. The comprehensive approach facilitated the exploration of potential comorbid conditions and the exclusion of other mood disorders or medical conditions that might mimic depressive symptoms. Client D.A. reported that her symptoms began in 2021 after learning of her romantic partner’s engagement to another woman. The SCID-5 depression module also included an examination of suicidal ideation, plans, and intent, although the client did not exhibit psychotic features. The severity specifier indicated the level of impairment, guiding treatment planning and intervention strategies. This instrument has been used in Nigeria by Okeafor and Okeafor[14] among patients with stroke in Nigeria.
MMPI-2: The MMPI-2, developed by psychologists McKinley and Hathaway in 1943 and revised in 1989,[15] is a comprehensive assessment tool designed to evaluate a wide range of psychological conditions and personality attributes, including psychopathologies such as depression, schizophrenia, and anxiety disorders. The MMPI-2 consists of 565 true-false items designed primarily for use with adults, providing an in-depth understanding of the client’s personality and aiding in the development of targeted treatment plans. It is widely used for clinical diagnosis, treatment planning, and psychological research, typically administered by trained mental health professionals like psychologists and psychiatrists. The MMPI-2’s psychometric properties are well established, demonstrating high reliability and validity. In Nigeria, the MMPI-2 has been utilized by clinical psychologists and researchers to assess and understand mental health issues within the Nigerian population, with adaptations to ensure cultural relevance and effectiveness. For instance, Tolulope et al.[16] used the MMPI-2 among patients in a psychiatric hospital in Benin, Nigeria.
The client’s scores on the Trin and Vrin scales fall within the acceptable range, indicating a valid profile and suggesting the client approached the assessment with consistency and sincerity. Elevated scores on the F, FB, and FP scales (t-scores 106, 101, and 98, respectively) suggest potential issues with test-taking attitude. High elevations may indicate severe psychopathology or a tendency to present oneself in an overly negative light. The client scores on the L, K, and S scales (t-scores 47, 33, and 30, respectively) fall within the acceptable range, indicating a valid profile and suggesting that the client did not approach the assessment with excessive defensiveness.
Elevations were noted on all clinical scales, particularly on the psychotic personality scales. This indicates the presence of gross psychopathology, suggesting significant psychological distress and dysfunction. The client’s personality falls into the 8-7/7-8 code type. Individuals with this code type may experience a great deal of turmoil, exhibit hesitancy in admitting psychological problems, and lack effective defenses against discomfort. They may manifest symptoms such as depression, anxiety, tension, and poor judgment. Given the elevated scores on various scales, neurotic, psychotic, and personality disorder diagnoses are equally likely. There is an increased likelihood of a psychotic diagnosis, even in the absence of clear psychotic symptoms, as such symptoms may not be overtly present.
Rotter incomplete sentence blank—college form: The Rotter Incomplete Sentences Blank (RISB)—College Form was developed by Rotter.[17] It measures an individual’s personality and emotional functioning by analyzing responses to incomplete sentences. The test is used to assess areas such as attitudes, motivations, and conflicts, providing insight into an individual’s psychological state. It is commonly used by clinical psychologists, counselors, and other mental health professionals in therapeutic and research settings. The RISB consists of 40 sentence stems that the respondent completes, with their responses being qualitatively analyzed for themes and quantitatively scored for overall adjustment. The test has demonstrated good reliability and validity, making it a useful tool for assessing psychological well-being in college students. This instrument has been used in Nigeria by Tamuno-opubo et al.[18] on a 16-year-old client.
The RISB results suggest that Client D.A. experienced significant regret, worry, and emotional distress related to her past failures, unmet needs, and plans, particularly regarding marriage. She has a deep-seated fear of losing everything and expressed feelings of depression, inadequacy, loneliness, and helplessness, alongside intense self-directed rage over past mistakes. Client D.A. perceives marriage as unattainable.
Draw-a-person: The DAP test, developed by Goodenough[19] and later expanded by Harris,[20] is a projective personality assessment tool that evaluates an individual’s psychological state based on their drawing of a human figure. It measures aspects of personality, emotional functioning, and cognitive development through the analysis of drawing features such as detail, proportions, and overall quality. Used primarily by clinical psychologists, school psychologists, and counselors, the DAP test involves asking the subject to draw a person, which is then interpreted using standardized scoring systems. This instrument has been used in Nigeria by Tamuno-opubo et al.[21] on assessment and management of conduct disorder of a 12-year-old.
The DAP test indicates that Client D.A. is highly sensitive about her appearance and exhibits aggressive and socially dominant behaviors as a compensatory defense mechanism for her feelings of inadequacy. She appears reluctant to engage with others, showing signs of evasiveness and possible maladaptive withdrawal, suggesting unease in social situations. Together, these results imply that Client D.A. struggles with profound emotional and social challenges, including potential depression, low self-esteem, and social anxiety.
Case conceptualization: Client D.A. is a 32-year-old unmarried female reported to have experienced persistent low mood, changes in sleep patterns, disruptions in appetite, feelings of worthlessness, and social withdrawal. The symptoms have been present for approximately two years, significantly impacting her daily functioning and overall quality of life. She reported a history of loneliness, feeling inferior, unimportant, and catered to by her caregivers. She also described a history of strained interpersonal relationships and distant family connections, suggesting a possible impact of early life stressors on her current mood. She also reported a lack of close social connections, leading to feelings of isolation and exacerbating the impact of the depressive symptoms. She stated that the abrupt end of her love relationship triggered the onset of her depressive episode approximately two years ago.
The client engaged in frequent negative self-talk and tended to interpret situations in a pessimistic and self-deprecating manners. Common cognitive distortions, including overgeneralization and catastrophizing, contributed to the maintenance of depressive symptoms. Her withdrawal from social interactions perpetuated a cycle of isolation, limiting positive reinforcement and support opportunities and bringing about “innovative helplessness”; “innovative helplessness” in the context of depression refers to a state in which the individual feels imprisoned in their condition. The client lacks the ability to explore novel strategies or ways to alleviate their symptoms. Individuals may experience a sense of being overwhelmed by their depressed moment, resulting in feelings of hopelessness and a reluctance to explore new strategies for managing their condition or seeking assistance. This can perpetuate the cycle of depression and hinder the individual’s ability to overcome their negative thoughts and behaviors.
Client D.A. was assessed for eligibility for treatment using the SCID-5, MMPI-2, RISB, and DAP. Following the initial assessment, she was assigned to treatment and evaluated psychologically regularly. In order to overcome this situation, it is necessary to motivate the client to question their ideas regarding their capacity to bring about change.[22] It is crucial to offer them assistance and access to resources that enable them to investigate novel therapeutic alternatives and coping mechanisms.
Course of treatment: The treatment plan for Client D.A. was developed based on the comprehensive assessment, including the SCID-5, MMPI-2, RISB, and DAP tests. This multifaceted approach aimed to address the biological, psychological, and social factors contributing to her depressive symptoms, ultimately enhancing her overall well-being. Cognitive behavioral therapy (CBT) was a central component of the treatment plan. The primary objective of CBT was to identify and restructure negative thought patterns and cognitive distortions that perpetuated Client D.A.’s depressive symptoms. Techniques were introduced to challenge and modify these negative thoughts, promoting a more balanced and positive outlook. Additionally, CBT helped reintroduce previously enjoyed activities to restore a sense of fulfillment in her life. IPT was also incorporated to address the social isolation and strained interpersonal relationships that Client D.A. experienced. The therapy focused on improving her communication patterns, managing role transitions, and resolving interpersonal conflicts. This approach was crucial in rebuilding her social network and reducing feelings of loneliness.
Pharmacotherapy (fluoxetine, amitriptyline) was included to address the neurobiological factors contributing to MDD. In collaboration with a psychiatrist, appropriate antidepressant medication was prescribed for Client D.A. Regular follow-up appointments were scheduled to monitor her response to the medication, manage any side effects, and ensure adherence to the treatment regimen. To help manage stress and anxiety symptoms, mindfulness and relaxation techniques were introduced. Techniques such as mindfulness meditation and progressive muscle relaxation were implemented to assist Client D.A. in managing her anxiety and improving her overall sense of well-being. She was urged to acknowledge the significance of social support and engage in activities such as reconnecting with family members and participating in support groups or community activities as part of the treatment plan. This aimed to foster social connections and reduce isolation, providing her with a stronger support network.
Finally, developing a structured daily routine was emphasized to establish a healthy and balanced lifestyle. The routine prioritized self-care activities, physical exercise, and healthy sleep patterns. Additionally, activities that brought joy and a sense of fulfillment were integrated into her daily life, promoting a more positive and structured approach to her daily activities. The holistic treatment plan was designed to target and reduce the severity of depressive symptoms, increase social engagement, and rebuild interpersonal relationships. By enhancing her coping mechanisms and equipping her with effective strategies to manage stressors, the treatment plan aimed to guide Client D.A. toward symptom relief and improved mental well-being. Regular evaluation and revision of the treatment plan were essential to ensure its relevance and effectiveness in meeting her specific needs.
Throughout therapy, Client D.A. experienced a gradual reduction in depressive symptoms, including improved mood, better sleep patterns, and increased social engagement. She consistently provided feedback during weekly sessions, which was documented and used to assess emotional and functional progress. This feedback, collected through self-report questionnaires and reflective discussions, was crucial in adjusting interventions to meet her evolving needs. By mid-treatment, Client D.A. acknowledged that CBT helped her challenge negative thought patterns and re-engage in previously enjoyed activities, while IPT facilitated better communication with family members, reducing her sense of isolation. Mindfulness techniques also contributed to decreased anxiety and stress. The combined use of CBT and IPT effectively addressed her cognitive distortions and social isolation, with pharmacotherapy alleviating biological symptoms such as fatigue and insomnia. Progress was regularly monitored using the Hamilton Depression Rating Scale (HDRS), with ongoing improvements in her emotional and functional well-being.
DISCUSSION
Results: A comprehensive evaluation of Client D.A. revealed a clinical diagnosis consistent with MDD. The assessment included the SCID-5 depression module, the MMPI-2, and projective tests such as the RISB and the DAP test. Each tool contributed to a detailed understanding of the client’s symptoms, severity, and impact on daily functioning.
Based on the DSM-5 criteria, the SCID-5 evaluation confirmed the diagnosis of MDD. Client D.A. reported persistent low mood, altered sleep patterns, changes in appetite, feelings of worthlessness, and social disengagement. These symptoms have been present for approximately two years, significantly impairing her daily functioning and overall quality of life.
The MMPI-2 provided a comprehensive assessment of Client D.A.’s personality and psychological state. Elevated scores on the F, FB, and FP scales indicated potential issues with test-taking attitude, suggesting severe psychopathology or a tendency to present herself in an overly negative light. Despite this, her scores on the L, K, and S scales fell within the acceptable range, indicating that she approached the assessment with consistency and sincerity. Elevated scores on various clinical scales, particularly the psychotic personality scales, suggested significant psychological distress and dysfunction. The client’s personality fell into the 8-7/7-8 code type, characterized by turmoil, hesitancy in admitting psychological problems, and a lack of effective defenses against discomfort. This profile indicated an increased likelihood of a psychotic diagnosis, even in the absence of overt psychotic symptoms.
The RISB results revealed significant emotional distress, marked by deep regret, worry, and feelings of inadequacy, loneliness, and helplessness. Client D.A. experienced profound sadness related to past failures and unmet needs, particularly concerning marriage, and harbored intense self-directed anger. These findings suggested a high risk of depression and severe self-esteem issues, indicating the need for therapeutic interventions focused on cognitive restructuring, emotion regulation, and developing a more positive self-concept.
The DAP test indicated that Client D.A. exhibited a heightened sensitivity about her appearance and employed aggressive and socially dominant behaviors as compensatory defenses against her feelings of inadequacy. Her reluctance to engage with others and her tendency toward evasive and maladaptive withdrawal suggested significant social anxiety and discomfort in social situations. These implications pointed to the need for therapies that enhance social confidence and reduce avoidance behaviors, such as cognitive-behavioral therapy and IPT.
By the conclusion of the intervention, measurable improvements were observed in Client D.A.’s depressive symptoms. Her HDRS score decreased from 22 (severe depression) to 8 (mild depression), and she reported enhanced social connections and increased participation in family activities. Follow-up assessments highlighted improved sleep patterns, reduced feelings of worthlessness, and a renewed sense of purpose. Her emotional and social functioning improved considerably, with notable progress in interpersonal relationships confirmed through self-reports. The comprehensive assessment, incorporating the SCID-5, MMPI-2, RISB, and DAP tests, revealed the multifaceted nature of her depression and informed the development of a holistic treatment plan. Client D.A. also experienced a return to work, increased social interactions, and a greater sense of fulfillment, with her feedback indicating heightened optimism and strengthened family relationships.
Objective assessment tools and self-reported progress confirmed a marked improvement in mental and social functioning. The examination highlighted many predisposing, precipitating, perpetuating, and protective factors that contributed to the client’s depressive episodes, in addition to the diagnostic confirmation as shown below:
A multimodal treatment strategy for MDD was developed with the goal of addressing the nature of the client’s symptoms. By linking the identified issues to specific interventions, the treatment plan aims to alleviate depressive symptoms, improve social functioning, and develop effective coping mechanisms. The integrated approach, combining therapeutic, pharmacological, and behavioral treatments, guides the client in her journey toward symptom relief and overall mental well-being. Regular evaluation and revision of the treatment plan ensure that it remains relevant and effective in meeting the client’s specific needs.
CONCLUSION
Client D.A.’s case study highlights the complex interplay of biological, psychological, and social factors contributing to her MDD. A comprehensive assessment using the SCID-5, MMPI-2, RISB, and DAP tests provided valuable insights into her symptoms and stressors, confirming the diagnosis and informing a holistic, culturally sensitive treatment plan. The multimodal approach, incorporating CBT, IPT, pharmacotherapy, and mindfulness practices, successfully addressed the biological, psychological, and social dimensions of her depression. Regular monitoring and collaboration with a psychiatrist ensured the treatment remained effective and relevant. By the conclusion of the intervention, measurable improvements were observed, with her depressive symptoms reducing from severe to mild on the HDRS. Client D.A. reported enhanced mood, better sleep patterns, increased social engagement, improved self-esteem, stronger interpersonal relationships, and a more optimistic outlook. This case underscores the importance of individualized, culturally tailored treatment approaches, particularly for clients with complex symptomatology. The progress observed in Client D.A. reinforces the value of integrated therapeutic strategies that address biological, psychological, and social factors, focusing on cultural sensitivity and personalized care to maximize therapeutic outcomes.
Authors’ contributions
TTA served as the supervisor and therapist, AOO clerked the patient, JOO administered and interpreted test instrument. All authors were involved in the following and clinical proceedings.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Well-Being and Mental Wellness. Oxford Research Encyclopedia of Global Public Health; 2020.
- World Health Organization (WHO). Depressive Disorder (Depression): Overview. 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/depression/?gad_source=1&gclid=CjwKCAjwx-CyBhAqEiwAeOcTdckIdJyU55KzxwgTgtJ6TdKY5OjfDlCn5cFRmakg8u8oFVLFZM9NWRoCPuEQAvD_BwE [Last accessed on 2024 September 15]
- Cognitive Therapy for Chronic and Persistent Depression. John Wiley & Sons; 2004.
- Adelowo OF. Logotherapy and Cognitive Behavioural Therapy in the Treatment of Depressive Disorder Among Stigmatised People Living with HIV/AIDS in Oyo State, Nigeria (Doctoral Dissertation); 2023.
- Zwart, R. Experiences of Depression in Black South African Young Adult Men in the Workplace (Master’s Thesis, University of Pretoria (South Africa)); 2020.
- Surviving Mental Illness: Stress, Coping, and Adaptation. Guilford Press; 1993.
- Being Treated Differently: Stigma Experiences with Family, Peers, and School Staff Among Adolescents with Mental Health Disorders. Soc Sci Med. 2010;70:985-93.
- [CrossRef] [PubMed] [Google Scholar]
- Anyaelesim CMP. Factors Contributing to Depression in Adolescent Admitted in a Psychiatric Hospital. Signature 2019. Available from: https://uir.unisa.ac.za/bitstream/handle/10500/25733/dissertation_anyaelesim_cmp.pdf;sequence=1
- Determinants of obstructed labour and associated outcomes in 54 referral hospitals in Nigeria. BJOG: An International Journal of Obstetrics & Gynaecology 2024
- [PubMed] [Google Scholar]
- Reciprocal Links Among Differential Parenting, Perceived Partiality, and Self-worth: A Three-wave Longitudinal Study. J Fam Psychol. 2005;19:633-42.
- [Google Scholar]
- Community based Multi-centric Service Oriented Research on Mental Illness with Focus on Awareness, Prevalence, Care, Acceptance and Follow-up in Bangladesh. Manual on Mental Health for primary health care physicians 2007
- [Google Scholar]
- Cognitive Behavior Therapy for Depression: A Case Report. Journal of Clinical Case Rep. 2018;8:2.
- [Google Scholar]
- The Structured Clinical Interview for DSM-5 Disorders (SCID-5). American Psychiatric Publishing; 2013.
- PHQ-9 Diagnostic Accuracy and Optimal Cut-off for Depression Among Patients with Stroke in Nigeria. Ann Ib Postgrad Med. 2023;21:11-6.
- [Google Scholar]
- The Identification and Measurement of the Psychoneuroses in Medical Practice: The Minnesota Multiphasic Personality Inventory. J Am Med Ass. 1943;122:161-7.
- [Google Scholar]
- Patterns of MMPI-2 Code Types in a Psychitric Hospital in Nigeria. IFE PsychologIA: An Int J. 2018;26:3-8.
- [Google Scholar]
- Rotter JB. The Rotter Incomplete Sentences Blank; 1950.
- Assessment and Management of Depressive Disorder of an Adolescent: A Case Report of 16-year-old Client. Ife Soc Sci Review. 2023;31:139-45.
- [Google Scholar]
- Measurement of Intelligence by Drawings. World Book Company; 1926.
- Harris DB. Children’s Drawings as Measures of Intellectual Maturity: A Revision and Extension of the Goodenough Draw-a-Man Test. (No Title).
- Case Report on Assessment and Management of Conduct Disorder of a 12-year-old. Eval Stud Soc Sci. 2023;4:41-53.
- [Google Scholar]
- Impact of the Brave Heart Mental Health Intervention on the Prevalence and Severity of Depression Among Young Internally Displaced Persons in Northern Nigeria. Journal of Medicine, Surgery, and Public Health. 2024;2:100053.
- [CrossRef] [Google Scholar]








