Translate this page into:
Ruptured Cerebral Abscess Presenting as Catatonia: A Case Report
*Corresponding author: Dr. Apurba Narayan Mahato MD, Department of Psychiatry, Central Institute of Psychiatry, Kanke, Ranchi, India. apurbanm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahato AN, Patel N, Mudaliyar S. Ruptured Cerebral Abscess Presenting as Catatonia: A Case Report. Acad Bull Ment Health. 2024;2:42-4. doi: 10.25259/ABMH_1_2024
Abstract
Catatonia is a complex syndrome having both neurological and psychiatric manifestations. It has a long history of connection with psychiatric illnesses. Despite being a distinctive clinical syndrome, catatonia often goes unrecognized in both psychiatry and neurology clinics. In the following case report, we demonstrate a case of a massive ruptured brain abscess, presenting primarily as catatonia.
Keywords
Catatonia
Cerebral abscess
Catatonia due to secondary medical conditions
INTRODUCTION
Catatonia as a separate diagnostic entity was first proposed and described by Karl Ludwig Kahlbaum in his book Catatonia, or tension insanity published in 1874.[1] Kahlbaum attributed the condition to organic cerebral disease and nowhere equated this with any specific mental illness. But over the next few decades, catatonia got quite wrongly associated with mental illnesses, more specifically schizophrenia.[2] Emil Kraepelin did not consider catatonia an independent neuropsychiatric syndrome or a complication of many different illnesses. He believed that catatonia was a basic presentation of dementia praecox, alongside hebephrenia and paranoid dementia.[3] This notion was carried forward later by Eugene Bleuler, too, and until the late 1900s, Catatonia had become only a subtype of schizophrenia.[2, 3] This concept continued till the 10th version of the International Classification of Diseases (ICD-10), where catatonia was mentioned only under catatonic schizophrenia. However, catatonia was later found to be more commonly seen in patients suffering from general medical and neurological conditions and mood disorders.[3–5] Neurological conditions presenting as catatonia are varied, that is, post status epilepticus, infective, neoplasms, autoimmune, metabolic encephalopathy.[6] Lesions at different brain regions have been found to be associated with catatonia (frontoparietal lobe, corpus callosum, basal ganglia), and diffuse brain lesions are more significantly associated than focal ones.[7] On the neurotransmitter level, dysregulation in Gamma Aminobutyric acid type A (GABA-A), Glutamate, and Dopamine pathways have been implicated.[8]
Despite being a distinctive clinical syndrome, catatonia often goes unrecognized in both psychiatry and neurology clinics. Here, we present a rare case of a massive ruptured brain abscess presenting as catatonia.
CASE REPORT
Our patient, a 37-year-old female, was brought to the OPD with chief complaints of on and off low mood, self-muttering, and aloofness for five years, and sudden onset change in behavior, evident by maintaining postures for long, mutism, and unprovoked agitation for 20 days. In the last two days, she was walking unsteadily and was tending to fall. Medical history included pulmonary tuberculosis 18 years ago, which was inadequately treated. Family history was insignificant except for probable Alzheimer’s dementia with behavioral symptoms in the patient’s father starting at the age of 69 years. She had already been diagnosed with schizophrenia and depressive illness with psychotic features several times and received treatment consisting of antipsychotics (risperidone, quetiapine, and clozapine) and antidepressants (Sertraline and amitriptyline). She last consulted with a psychiatrist a week before presenting to our hospital, where the antipsychotic dose was increased without any response. At presentation, she had mutism, cataplexy, rigidity, negativism, perseveration, and asymmetric reflexes but no fever or unstable vitals. On examination, her orientations to time, place, and person were found intact after much effort, owing to her catatonic symptoms. A detailed cognitive assessment was planned once catatonic symptoms improved. A provisional diagnosis of secondary catatonia syndrome was made, with a differential diagnosis of catatonia associated with another mental disorder. Symptomatic management was urgently initiated and neuroimaging was sent for. CT scan report came the next day, which showed a massive cerebral abscess (suspected tubercular etiology) with recent rupture and expansion to the left lateral ventricle with midline shift (Figures 1a–1b). As soon as the CT was available, urgent neurosurgery consultation was taken, and she was started on a parenteral regimen of ceftazidime, metronidazole, dexamethasone, and mannitol. Blood for culture was taken prior to starting antibiotics. She was shifted to a neurosurgery unit, and burr hole decompression was planned. Despite aggressive supportive management, she succumbed to her illness on the same day before further evaluations and management could have been undertaken.

- CT Brain of patient on presentation: shows massive left sided ruptured abscess.
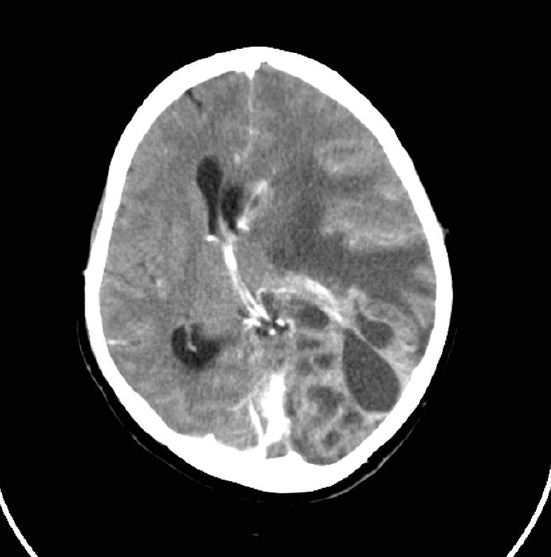
- CT Brain of patient on presentation: shows massive left sided ruptured abscess with mid-line shift.
DISCUSSION
Catatonia as a separate clinical syndrome has already been included in a recent major classification systems, that is, the latest 11th revision of the ICD-11[9] and the Diagnostic and statistical manual of mental disorders (DSM-5).[10] Further, Research Domain Criteria (RDoC) has also introduced a separate sensorimotor domain, which describes abnormalities of the sensorimotor and psychomotor domain associated with mental disorders.[11] Still, there is a considerable lack of consensus regarding the identification and management of catatonia as a distinct identity.
Here, in this case, it seems more likely that the catatonic presentation was unrelated to the psychosis. Initially, catatonia seemed to be an extension of psychotic symptoms, as she was already having a long history of psychosis. Prior to coming to us, she consulted a psychiatrist, who conceptualized the catatonic symptoms as a part of worsening psychotic symptoms and hiked the antipsychotic medication dosages. Only after the imaging we came to know that the reason for recent catatonia might be different. With the background of schizophrenia, the ruptured abscess seems to have set forth the recent onset of catatonia. Neuroleptic malignant syndrome could have been a differential, which was ruled out due to intact orientation, absence of fluctuating pattern of attention and orientation, hyperthermia, and autonomic instability.
CONCLUSION
This case report once again emphasizes the fact that we need to timely rule out all possible organic aetiologies before diagnosing a case presenting with catatonic symptoms as part of an ongoing mental illness such as schizophrenia.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligenceAI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Catatonia or Tension Insanity: A Clinical Form of Psychic Illness. Berlin: Verlag Aughust Hirschwald; 1874.
- Re-Awakening to a Forgotten Disorder. Movement Disorders. 1999;14:395-7.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia is not Schizophrenia: Kraepelin’s Error and the Need to Recognize Catatonia as an Independent Syndrome in Medical Nomenclature. Schizophrenia Bulletin. 2010;36:314-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Catatonia: Clinical Aspects and Neurobiological Correlates. J Neuropsychiatry Clin Neurosci. 2009;21:371-80.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia in Diagnostic and Statistical Manual of Mental Disorders. The journal of ECT. 2010;26:246.
- [CrossRef] [PubMed] [Google Scholar]
- Why do Neurologists Miss Catatonia in Neurology Emergency? A Case Series and Brief Literature Review. Clinical Neurology and Neurosurgery. 2019;184:105375.
- [CrossRef] [PubMed] [Google Scholar]
- Caroff SN, Mann SC, Francis A, Fricchione GL, eds. Catatonia: From Psychopathology to Neurobiology. American Psychiatric Pub; 2007.
- What Catatonia can Tell Us About “Top-Down Modulation”: A Neuropsychiatric Hypothesis. Behavioral and Brain Sciences. 2002;25:555-77.
- [CrossRef] [PubMed] [Google Scholar]
- Schizophrenia in ICD-11: Comparison of ICD-10 and DSM-5. Revista de Psiquiatría y Salud Mental (English Edition). 2020;13:95-104.
- [Google Scholar]
- Advancing Translational Research Using NIMH Research Domain Criteria and Computational Methods. Neuron. 2019;101:779-82.
- [CrossRef] [PubMed] [Google Scholar]








